Better care, better health, and lower health care costs
These are the goals of the Vermont Health Care Innovation Project (VHCIP). Vermonters both inside and outside state government are developing new technologies and processes for making health care not just less costly and more efficient, but more effective.
VHCIP coordinates policy and resources for health care reform statewide. With a $45 million dollar federal State Innovation Model (SIM) grant VHCIP funds proposals to improve health care delivery, to build health information technology and databases, and to test new models for paying providers. VHCIP has also drawn on input from ten stakeholders’ Work Groups in making policy recommendations at the state level. Six of those Work Groups are still in action.
Serving as a conduit between public and private actors in health care reform, VHCIP fosters collaboration among the Green Mountain Care Board, the Vermont Agency of Human Services, Medicaid, private health insurers, and health care providers in the state. From the largest medical center to the smallest private practice in Vermont, providers are invited to participate in health care reform.
The Triple Aim
The goals of VHCIP align with The Triple Aim. As defined by the Institute for Health Improvement, The Triple Aim is “the simultaneous pursuit of improving the patient care experience, improving the health of populations, and reducing the per capita cost of health care.” As the IHI insists, these ambitious goals can only be achieved through broad systematic changes in health care.
The Triple Aim seeks to improve the experience of patients by making health care delivery safe, effective, patient-centered, timely, efficient, and equitable. It focuses on population health, which “cannot be realized by health care systems acting alone, nor by solely delivering high-quality care at lower costs. Improving health is a challenge that requires the engagement of partners across the community to address the broader determinants of health,” according to the IHI. And it does not aim simply to curb the growth in health care costs, but rather to reduce the amount spent per capita on health care. The Triple Aim is designed to result in “fundamentally new systems contributing to the overall health of populations while reducing the cost to society.”
Project Impact: First Two Years
By August, 2015, VHCIP had already demonstrated a significant impact on hundreds of providers and hundreds of thousands of beneficiaries in Vermont.
Through initiatives improving health care delivery, Vermont’s SIM grant has already engaged 420 providers in a Learning Collaborative focused on care delivery and practice transformation. Additionally, the health care delivery projects funded by sub-grants have affected 692 providers and 281,808 Vermonters who receive health care.
So far, VHCIP-supported improvements in the infrastructure for gathering and communicating health data have involved 400 providers in Vermont.
The impact of payment model projects has been even more substantial. Through Vermont’s Medicaid Health Home program authorized by the Affordable Care Act, state supplement programs (SSP), administration and policy in mental health (APMH), and pay for performance (P4P), altogether 442,643 Vermonters have received the benefit of new payment models. That’s more than two-thirds of the state’s population.
Remaining Work to Do
To build on progress in transforming health care practice and improving population health, VHCIP will:
- Expand the Learning Collaborative to include providers beyond the Burlington, Rutland, and St. Johnsbury areas
- Continue to sustain the projects funded by sub-grants throughout Vermont
- Foster regional collaborations among providers
- Conduct micro-simulation modeling of demand
- Finalize the Population Health Plan
To continue building the health data infrastructure, VHCIP plans to:
- Continue efforts to improve data quality and to remediate information gaps
- Invest in telehealth pilot programs
- Design and implement health information registry and data warehousing solutions
- Invest in a shared care plan and/or a solution for uniform data transfer protocol
- Launch a System Event Notification Service
To continue transformation of health payment systems, VHCIP intends to:
- Implement the third-year stage of state supplement programs (SSP) for Medicaid and commercial health care payers
- Analyze the feasibility of Accountable Communities for Health and the All-Payer model
- Implement Bundled Medicaid Episodes of Care
- Establish a Home Health Patient Positioning System (PPS)
Areas of Focus
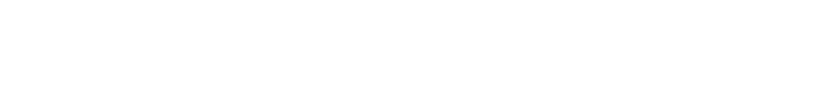
To achieve the Triple Aim of better care, improved health, and lower costs, VHCIP is designing and testing new systems for payment, care delivery, and information technology that will fundamentally change Vermont’s health care landscape. This means testing value-based payment models for all payers in the health care system; supporting providers as they prepare for increased accountability; and improving the infrastructure for collecting health data in Vermont. State government agencies and private organizations are working together to change policies and behaviors in order to transform the state’s culture of health care. VHCIP staff and contractors are charged with managing the project to ensure it is organized, has sufficient resources, and is able to meet goals and milestones.
Health Data Infrastructure
In order for providers, payers, and State agencies to be ready to participate in new payment models, Vermont’s health data infrastructure needs strengthening. VHCIP is investing in clinical data systems that will measure health care quality while at the same time supporting real-time decision making for clinicians. These systems measure quality passively, relieving providers of the burden of collecting data while still holding them accountable for quality.
VHCIP is also working to improve the ability of different information technology systems and software applications to communicate, to exchange data, and to use the data that has been exchanged. This interoperability will coordinate clinical data with insurance claims. It will also strengthen the state’s capacity for using predictive modeling, machine learning, and data mining to make predictions on the basis of facts.
Vermont’s Health Information Exchange (VHIE) has already benefitted from the project through the improved quality and quantity of data collected from providers’ electronic medical records. The VHIE is a secure computer network connecting the electronic health information of different providers to share clinical and demographic data of patients they share in common.
Payment Model Design and Implementation
Vermont has already established a nationally recognized patient-centered medical home (PCMH) program, the Blueprint for Health. A PCMH is a health care delivery model using teams of providers to improve health outcomes by giving patients coordinated and continuous care.
Building on the success of the Blueprint for Health and in accordance with the Affordable Care Act, Vermont launched Medicaid and commercial Shared Savings Accountable Care Organization (ACO) programs in 2014. Nearly 60% of Vermonters are participating in these two programs. The three ACOs in Vermont comprise the majority of the state’s health care providers, including many long-term services and support (LTSS) and mental health providers.
Now Vermont is designing and testing new value-based payment models to promote higher quality and more sustainable costs of health care. The new models being tested are pay-for-performance, episodes of care/bundled payments, prospective payment systems, and capitation (in which providers’ fees are determined by the number of patients served).
Some providers are more able to accept financial risk than others, so the payment models are designed to meet providers where they are. The models are intended to ensure that the State can evaluate the programs and the payers can make the new structure work. By establishing a path for all providers, Vermont is phasing in reforms broadly, but responsibly.
Vermont is also exploring an all-payer model, an agreement between the state and the federal government on a sustainable rate of growth for health care spending in that state. The agreement will include strict measurement of quality and performance. An agreement would also take into account all necessary Medicare waivers, the new structure of a global commitment waiver for Medicaid, and Vermont’s vision for the payment of providers.
Practice Transformation
VHCIP is working to help providers get ready to use alternative payment models and to accept higher levels of risk and accountability. Toward this end, VHCIP is monitoring Vermont’s existing health care workforce and designing activities to encourage practice transformation. Two successful initiatives have already come out of this effort, the VHCIP Sub-Grant Program and the Integrated Communities Care Management Learning Collaborative.
The Sub-Grant Program uses the federal SIM grant funds to support over 15,000 Vermont providers in their efforts toward practice transformation. Collectively, the sub-grant projects have had an impact on more than 300,000 Vermonters from all over the state.
The Integrated Communities Care Management Learning Collaborative seeks to improve care and reduce fragmentation for at-risk Vermonters and their families. Teams of health care and service providers from Burlington, Rutland, and St. Johnsbury have formed a VCHIP-sponsored Learning Collaborative to improve care delivery and population health for their regions. The goal of these pilot groups has been to intervene in the fragmentation, duplication, and gaps in care and services facing people with complex care needs. In the next phase, the Learning Collaborative will expand to include teams from the rest of Vermont.
Vermont’s Integrated Community Care Management Learning Collaborative has focused initially on the health care needs of at-risk populations, though the project will ultimately intervene in health care delivery for all Vermonters. Through periodic in-person and virtual learning sessions over the course of a year, the Collaborative identifies best practices for integrating care management (such as shared care planning, care management protocols for referrals, and transitions in care). The teams in each community identify existing gaps in services, determine the at-risk groups to receive new care management services, implement best practices, and test the innovations to measure success and accountability.
The immediate goals of the Learning Collaborative are to determine whether interventions improve care protocols, coordination of care and services, and communication among providers, as well as the care experience and outcomes for people who need services and for their families. The long-term goals for the Collaborative align with the Triple Aim: reducing per capita health care costs, improving care, and improving the health of Vermont’s population.
Evaluation
All federally supported SIM projects in Vermont are evaluated to ensure that the process and outcomes work for Vermont, for the state’s residents, for payers and for providers. Evaluations are conducted by program, by population, and by region. Evaluations are ongoing throughout the grant period, to anticipate unintended consequences and to help staff take action quickly on lessons that have been learned.
Evaluation tasks include the following:
- Developing and executing a Self-Evaluation Plan
- Doing surveys to measure patient experience and other factors, as identified in payment model development
- Taking action to monitor and evaluate activities within payment programs
The Evaluation Focus Area applies to the projects in the other three Areas of Focus: Health Data Infrastructure, Payment Model Design and Implementation, and Practice Transformation.